Racial Concordance: Why Clinical Trial Patients Need More Doctors Who Look Like Them
As clinical research professionals gather in Austin this week for the SCRS Diversity Site
Solutions Summit, it’s worth revisiting some of the research on how racial concordance impacts
healthcare and, by extension, clinical trials.
Racial concordance, when a patient and clinician have the same race or ethnicity, can improve
trust among populations where healthcare disparities are most prevalent. When a trusted
physician refers someone to a clinical trial, it increases the likelihood that they will participate,
improving the diversity of patient populations to ensure treatments are safe and effective for
everyone.
How does racial concordance impact healthcare?
Numerous research studies published over the past several decades highlight disparities and
systemic racism within the healthcare system. A 2003 report by the National Academies Press
analyzing patient and provider attitudes and behavior found racial and ethnic minority patients
received a lower quality of care than white patients even after accounting for differences in
income and insurance coverage. One study described in this report surveyed nearly 200
physicians about their own patients, including their degree of social support, how likely they
were to comply with medical advice, and even whether the physician could see themselves
being friends with them. The findings were troubling, revealing clear biases among the
physicians in the survey.
More recently, the Agency for Healthcare Research and Quality released a 2021 report that
showed although there had been substantial improvements in the quality of care for racial and
ethnic minorities in the past 20 years, there were lingering gaps. When asked about various
factors, including person-centered care, affordability and effective treatments, 43% of Black
patients, 40% of Native American patients, 36% of Hispanic patients, and 28% of Asian patients
still reported a lower overall quality of care compared to white patients.
The study also found the number of HIV-related deaths among Black patients were six times
higher than among white patients.
Additionally, despite a 48% overall decrease in end-stage renal disease due to diabetes from
2001 to 2018, Native American and Black patients still had higher rates of the disease
compared to white patients. For Hispanic patients, the incident rates were nearly double the
rates for white patients.
Research has found racial concordance can make a patient more likely to seek care, return for
visits and report greater satisfaction with their care.
At the same time, data shows found Black, Hispanic and Native American people are still
underrepresented among US physicians and healthcare professionals. One study of 2019
American Community Survey data found that while Black people represent approximately 12%
of the US working-age population, the rates of representation in 10 different healthcare
occupations ranged from only 3% to 11%. Similarly, Hispanic people are approximately 18% of
the working population, yet their representation among different occupations also ranged from
3% to 11%.
The Agency for Healthcare Research and Quality report also found only 11% of Black and
Hispanic patients and 20% of Asian patients reported racial concordant clinicians compared to
46% of white patients.
What do these findings mean for clinical trials?
Just as disparities still exist in healthcare, there is still a glaring lack of diversity when it comes
to who participates in clinical trials.
The same factors that make it more likely for patients to identify with and trust their physicians
may also make them more receptive to the idea of exploring a clinical trial as a care option.
Recruiting diverse patient populations is not only the right thing to do to ensure medications are
safe and effective for everyone; it’s now an FDA requirement.
Meeting enrollment goals outlined in the new Race and Ethnicity Diversity Plans can be
challenging, however, if patients don’t have a physician they trust who refers them to a trial.
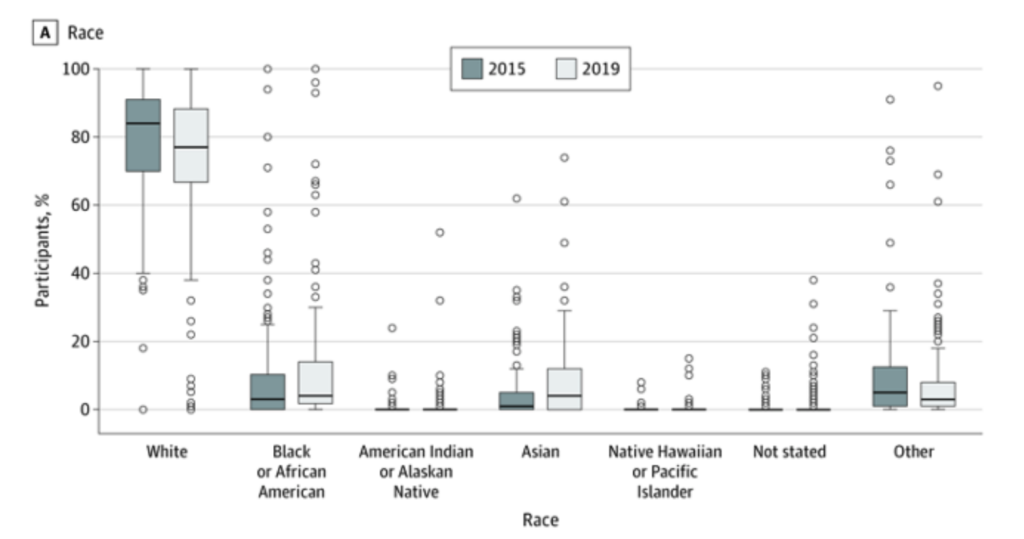
A cross-sectional study of all clinical trials published in major medical journals found
approximately 90% of all US trial participants were white in 2019. Other groups, including Black,
Native American and Asian populations, had much lower rates of participation.
 How can we improve racial concordance in clinical trials?
How can we improve racial concordance in clinical trials?
Having more physicians participate in clinical trials starts by acknowledging and addressing
barriers that may hinder them. Some of the biggest barriers to physician participation include a
lack of time, resources, and training. That starts by teaching every medical school student about
the benefits of clinical trial participation and how to conduct them.
Managing the logistics of a clinical trial can also be daunting without the right partnerships.
Patient recruitment is the most time-consuming aspect of most trials and the biggest cause of
delays. Marketing a clinical trial can be expensive if patient recruitment firms don’t have the right
data to effectively target eligible patients, and patients themselves may never be referred if they
don’t have a primary care physician they trust.
Improving racial concordance in healthcare goes hand in hand with improving diversity in clinical
trials.
At M&B Sciences, we believe a holistic approach is the best way to address this multifaceted
challenge. We work with hundreds of community organizations who have built trust among
diverse groups of people, including faith-based organizations and community-based
practitioners. Our expertise in spatial epidemiology also helps sponsors identify potential trial
participants faster and more cost effectively. Additionally, we’ve developed a program to train
naive investigators and support them through the clinical trial process in order to provide a new
onramp for community physicians interested in participating in clinical research.
We also believe in empowering patients by making clinical trials more accessible to them. While
our Neighborhood Trials app makes it easy for anyone to find a clinical trial close to home, the
platform provides another tool to help communicate this information to their patients, and helps
sponsors identify their targeted population for recruitment into clinical trials.
Learn more about how we can support your next clinical trial.